Platelet-Rich Plasma (PRP)
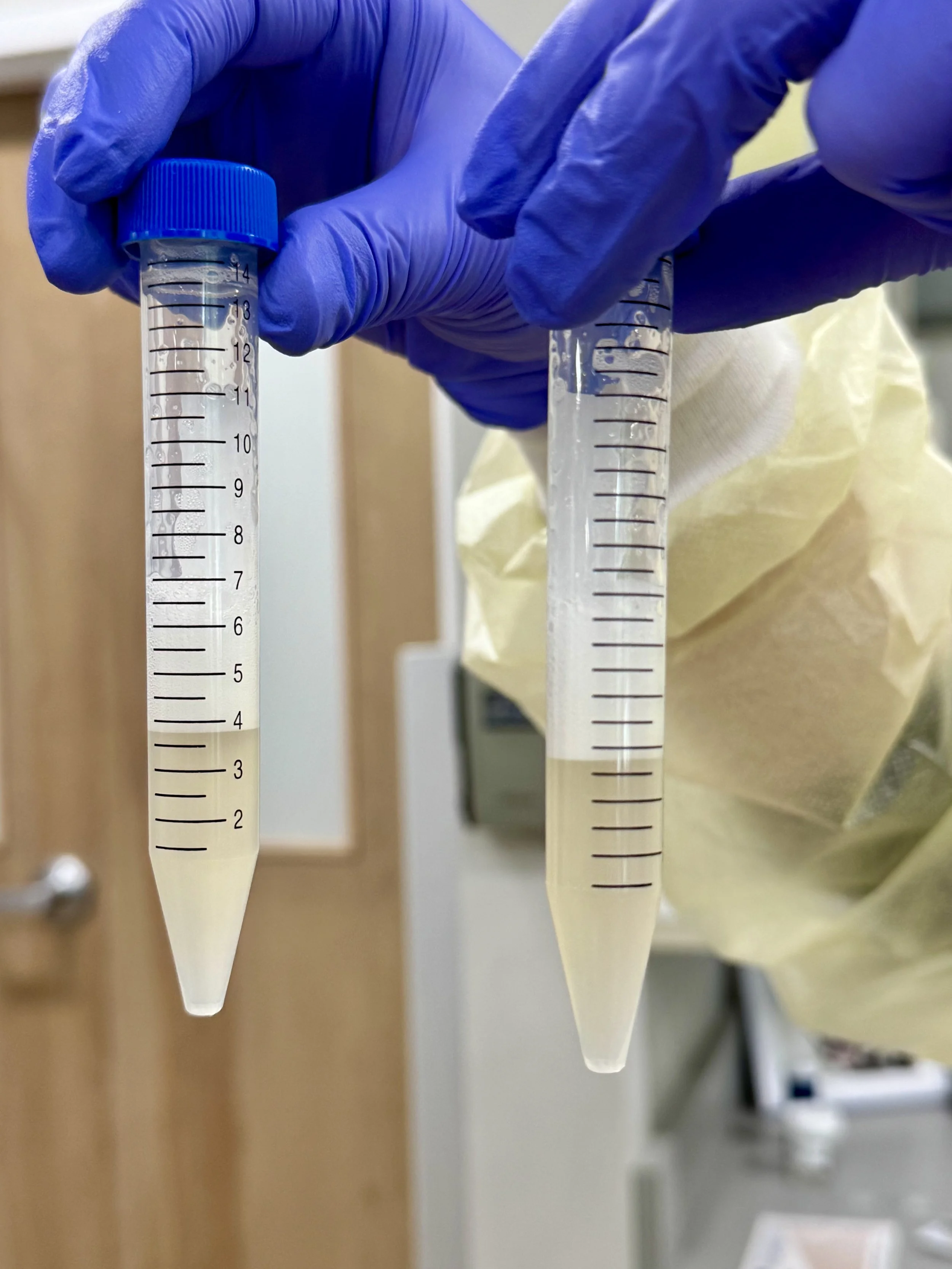
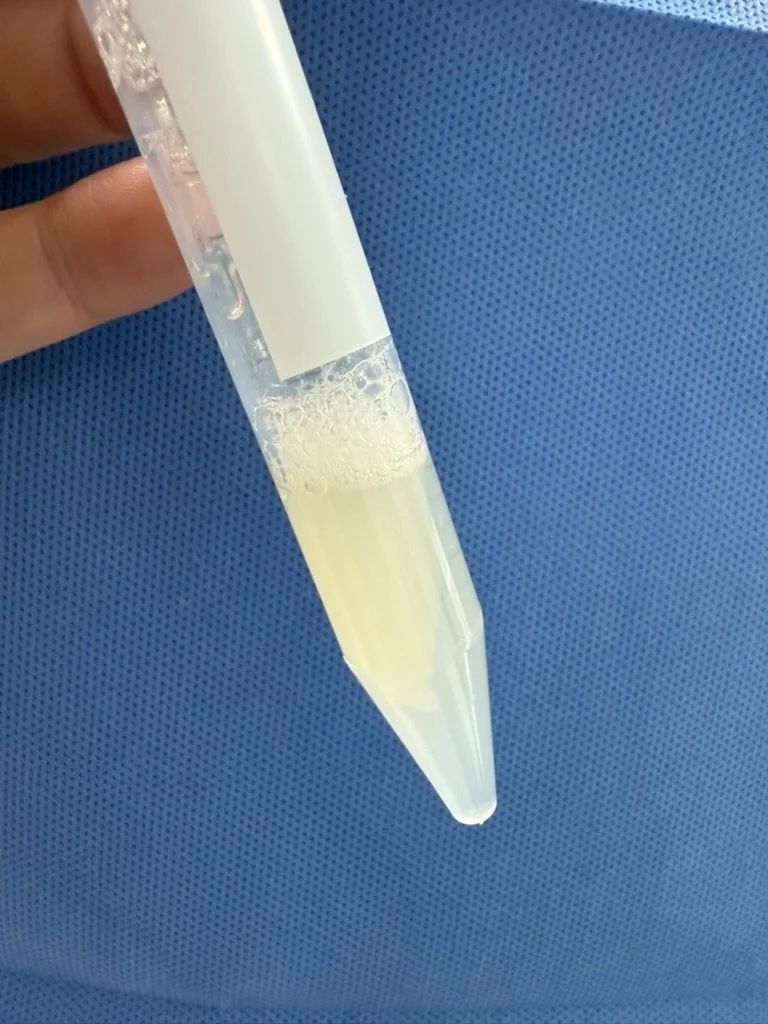
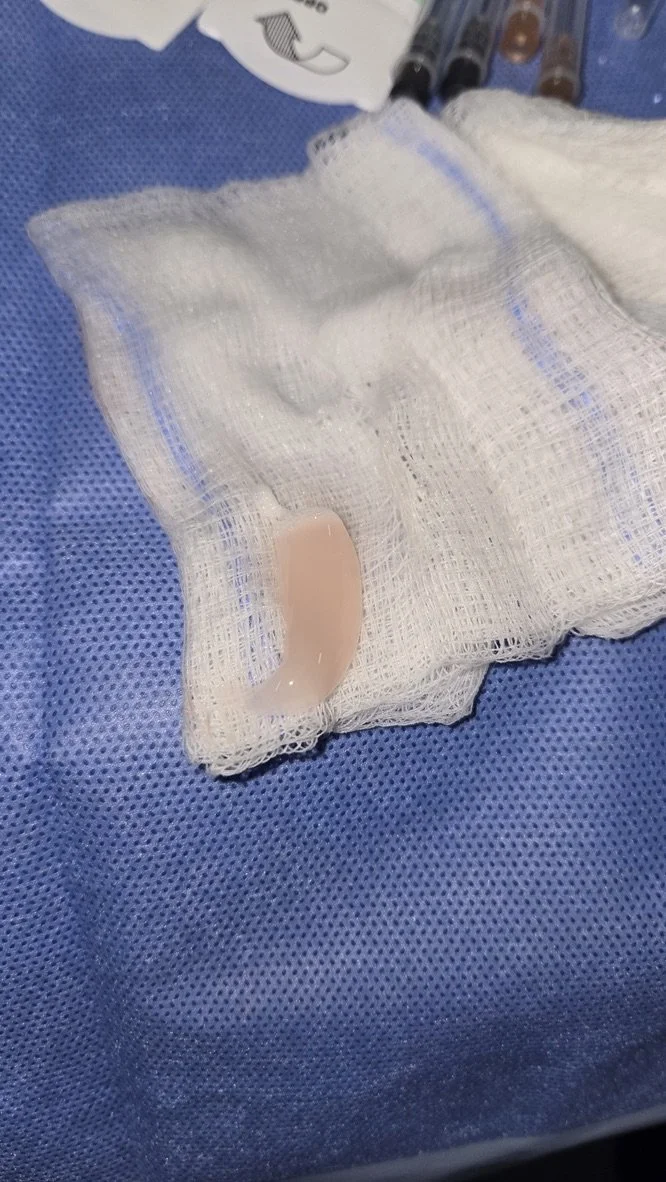
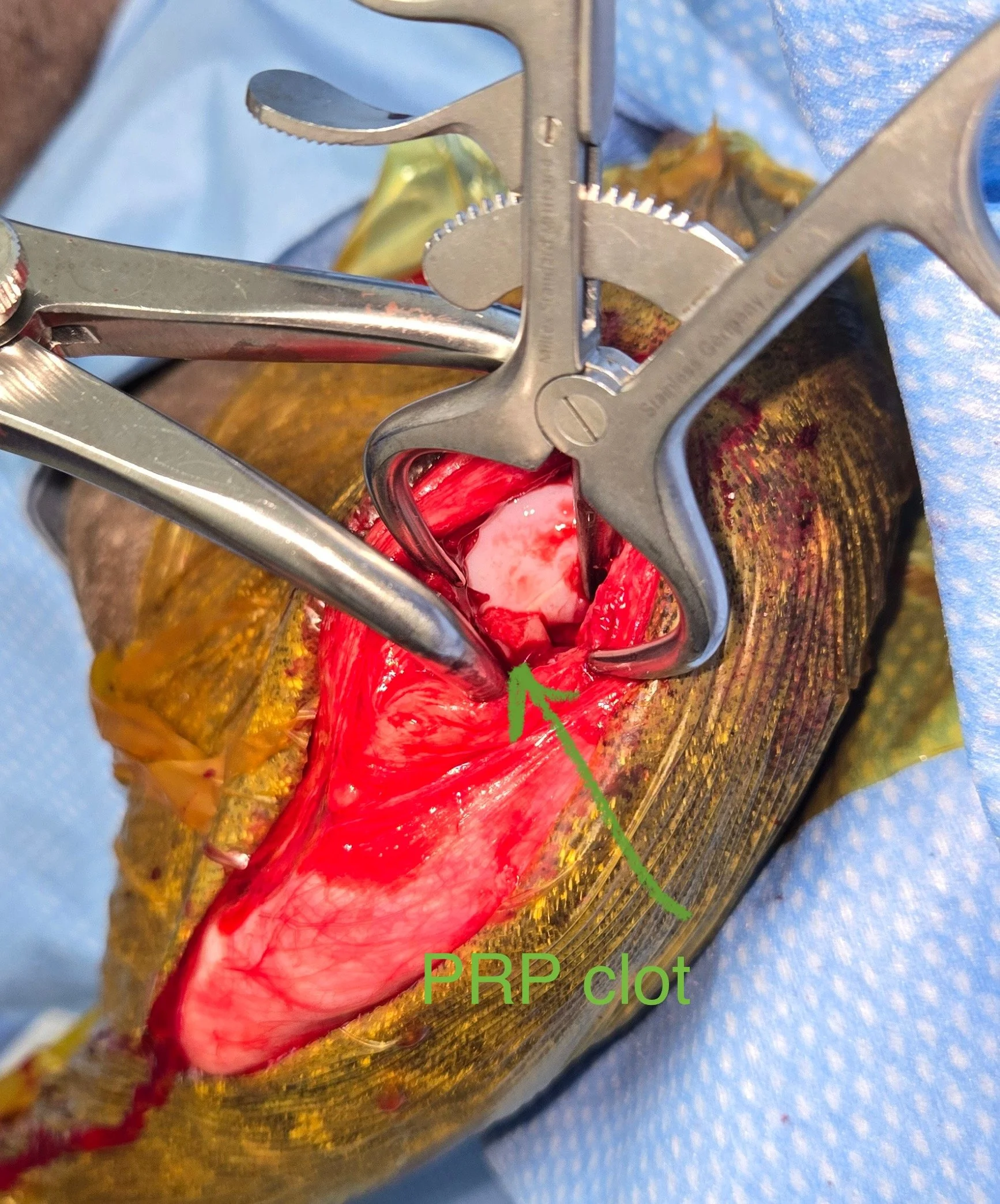
WHAT: Platelet-Rich Plasma or PRP is the platelet rich portion of blood after a series of centrifugations of whole blood. In more specific terms, PRP is a biological product containing the plasma fraction of autologous blood with a concentration of platelets and associated growth factors and cytokines that is higher than baseline (Carr, 2023). PRP is available as a liquid or in some systems as a semisolid clot (Ardent).
WHY: Platelets are first responders that migrate to the injury site and provide a critical hemostatic function. Platelets release growth factors that promote new blood vessel formation, trigger mitosis and macrophage activation, and increase collagen production from fibroblasts. Delivering PRP directly can help the tissue heal better and faster, with no risk of disease transmission or immune reaction because the patient’s blood is used.
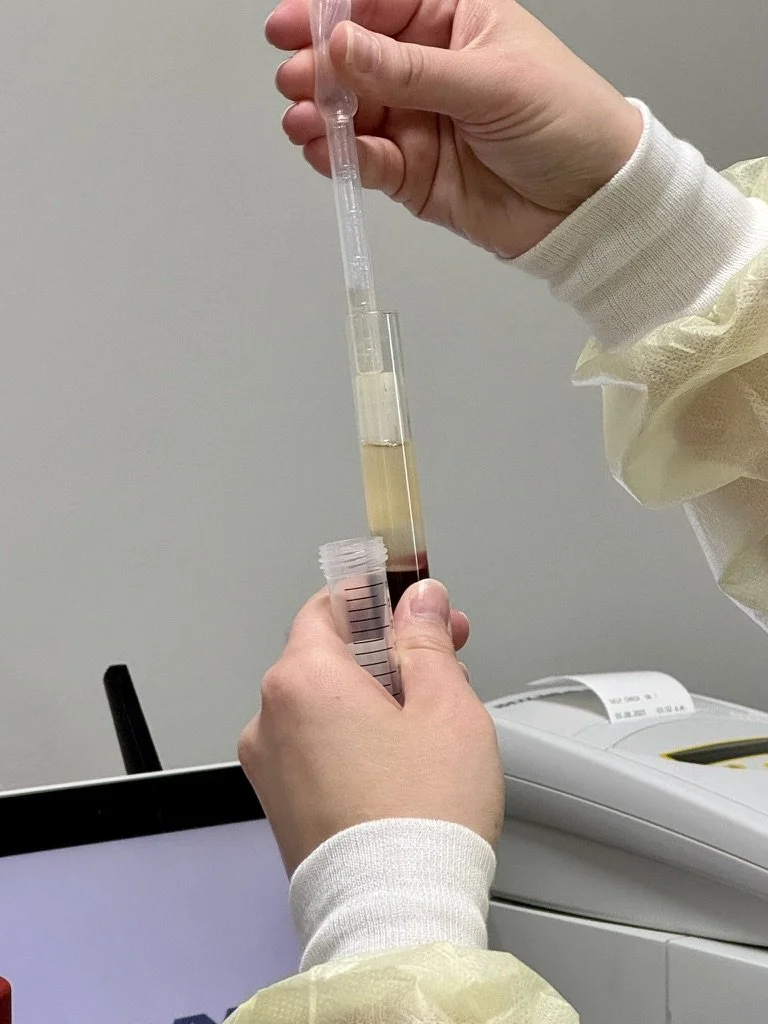
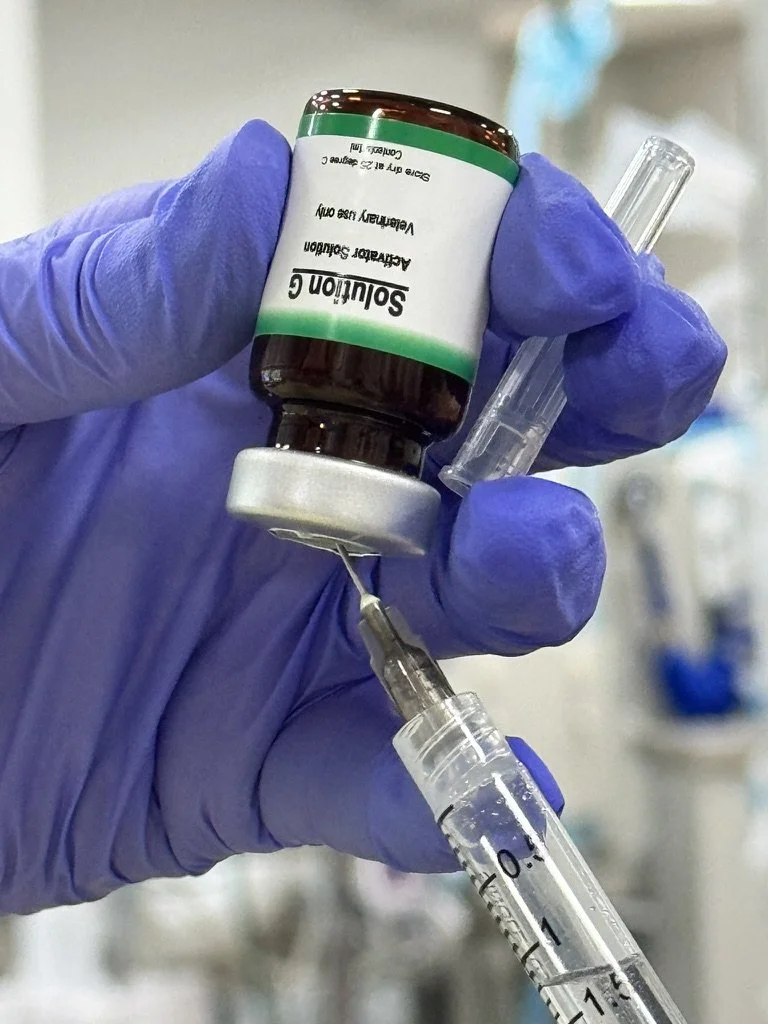
HOW: After the PRP layer is harvested, the platelets are then activated. Activation of the platelet triggers the release of its granules, including growth factor–rich alpha-granules. The associated growth factors and cytokines present in alpha-granules, which have been correlated to tissue healing include PDGF, TGF-α, TGF-β, VEGF, basic fibroblastic growth factor, epidermal growth factor, connective tissue growth factor, insulin-like growth factor, hepatocyte growth factor, and keratinocyte growth factor. These growth factors encourage cell recruitment, cell migration, cell proliferation, angiogenesis, and osteogenesis. PRP can work synergistically with stem cells by providing a scaffold and stimulating their regenerative and trophic potential.
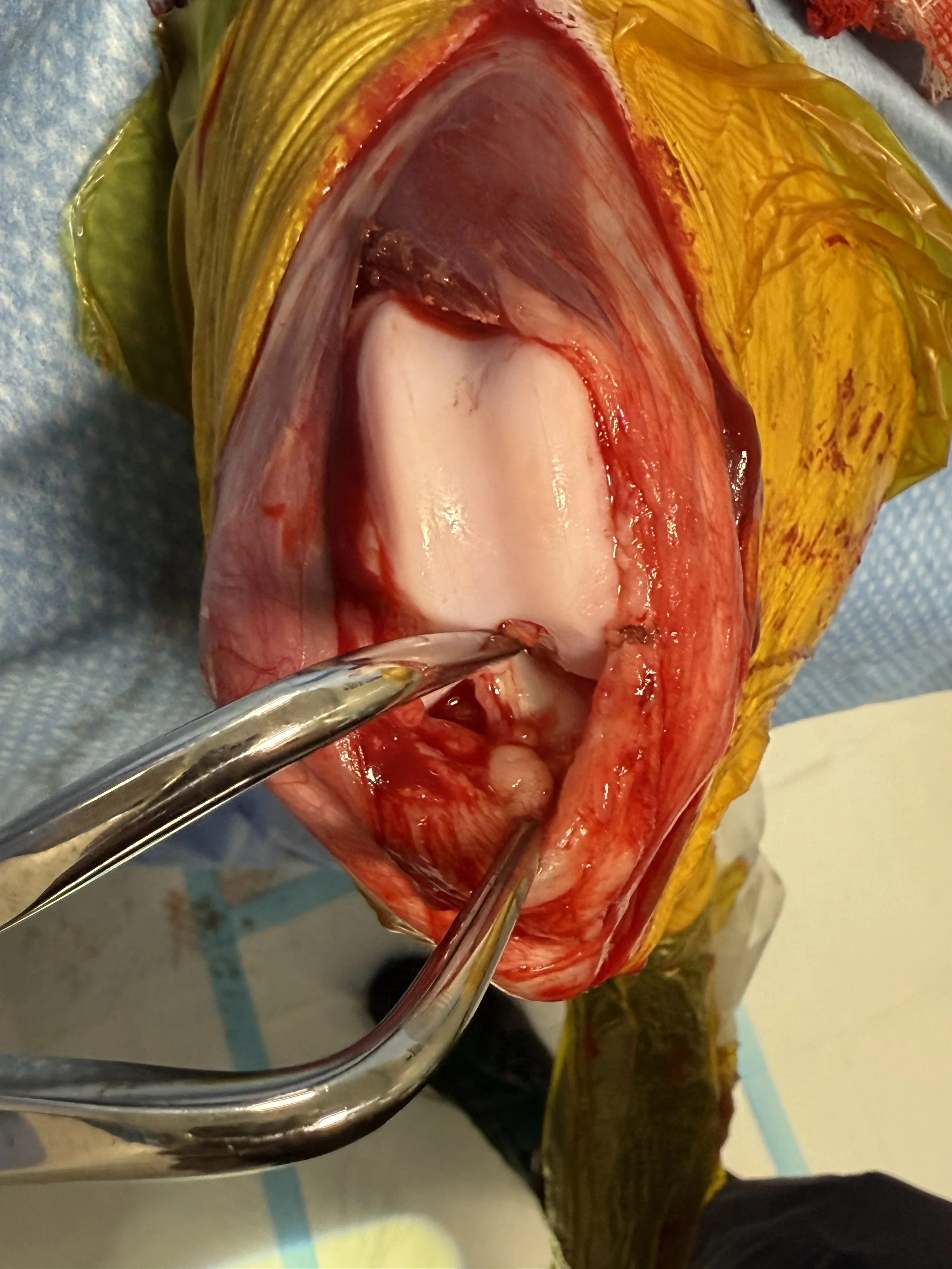
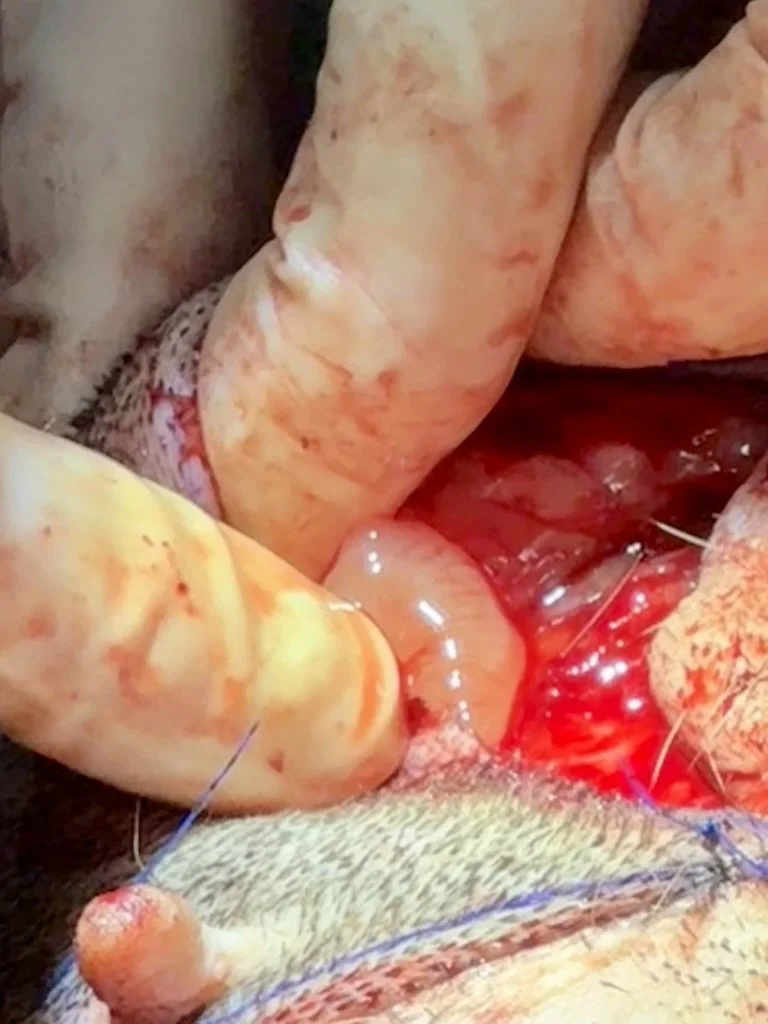
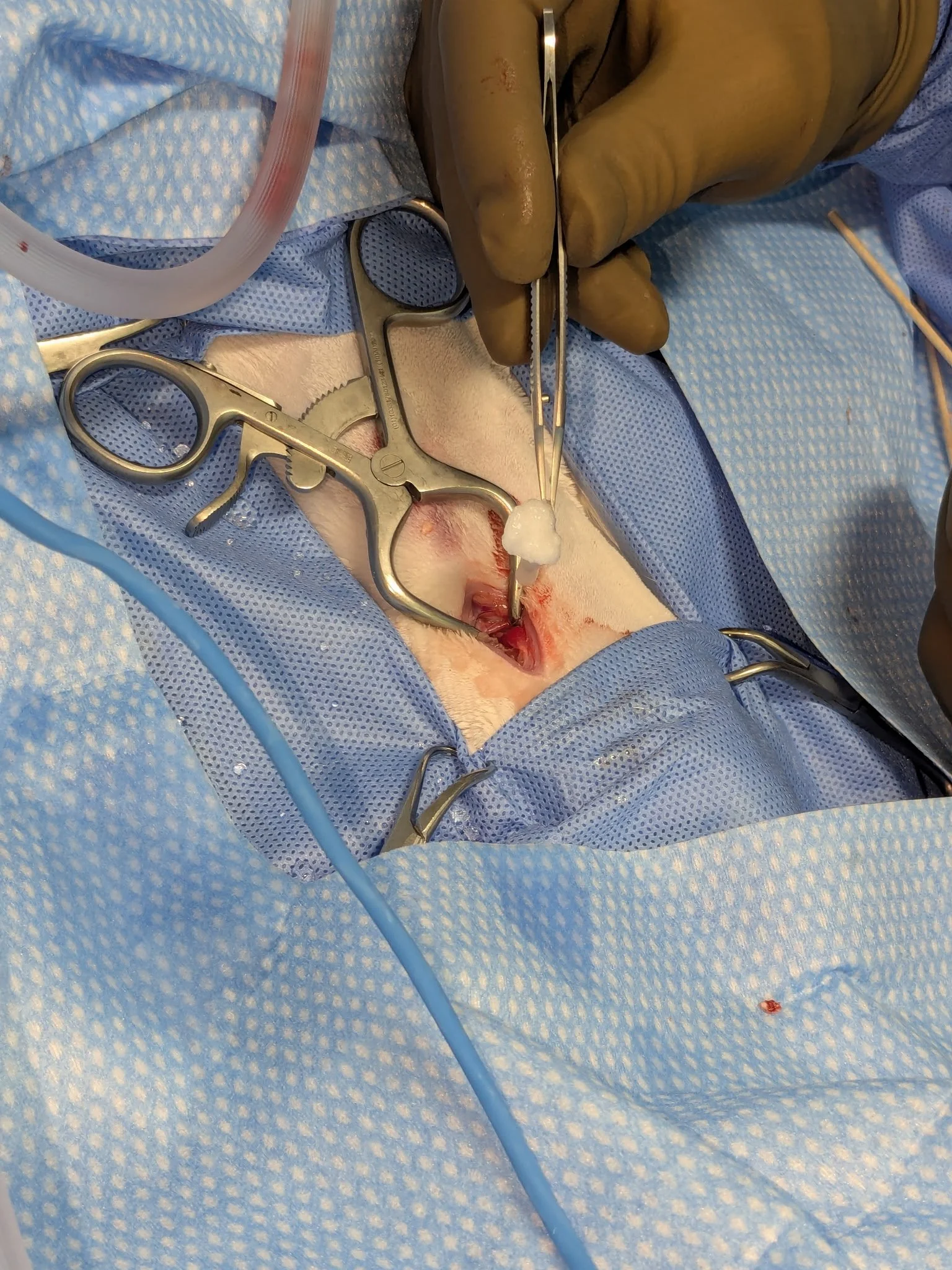
WHEN/WHERE: PRP can be used intrarticularly for arthritis, in wounds to promote healing, fracture sites, tendon injuries, to help fight infections and in arthrodesis sites. Currently it is recommended to avoid injecting in cancerous lesions.
The Process of PRP production
Applications of PRP